When you are asked to examine CVS, Cardiovascular system of a patient, always start from the general physical examination except when examiner asks you to omit it. Examination of the cardiovascular system consists of:
- Examination of pulse
- Measurement of blood pressure
- Examination of neck veins
- Examination of precordium by
- Inspection
- Palpation
- Percussion
- Auscultation
How to Examine Pulse?
Pulse is a wave imparted by the contraction of left ventricle to the blood column.
Commonly felt pulses are:
- Radial artery
- Brachial artery
- Carotid artery
- Femoral artery
- Popliteal artery
- Posterior tibial artery
- Dorsalis pedis artery
During Examination of the pulse, note the following features:
- Rate (60-100 beats/min)
- Tachycardia: pulse rate more than 100 per minute. Causes: exercise, fever, anemia, tachyarrhythmias, thyrotoxicosis, heart failure and hypotension.
- Bradycardia: pulse rate less than 60 per minute. Causes: Athletes, complete heart block, hypothyroidism, drugs like digoxin, and raised intracranial pressure.
- Rythm
- sinus arrythmia: normal phenomenon- pulse rate is faster in inspiration and slower in expiration. lost in heart failure and autonomic neuropathy.
- regularly irregular: premature beats occurring at fixed interval, e.g., after one normal beat (bigeminy) or two normal beats (trigeminy). Cause: digoxin toxicity
- irregularly irregular: there is no pattern, beats occur irregularly. Causes: atrial fibrillation, atrial flutter
- pulsus deficit: Difference between pulse rate and heart rate is called pulse deficit. It is found in atrial fibrillation, causes include: mitral stenosis, thyrotoxicosis, ischemic heart disease.
- Volume
- high volume: fever, aortic regurgitation
- low volume: heart failure, hypovolemic shock
- Comparison with other pulse
- radio femoral delay: in coarctation of aorta, femoral pulse is weak and delayed as compared to radial pulse.
- radio radial delay: Subclavian artery stenosis, aortic coarctation, aortic stenosis
- don’t palpate both carotids simultaneously
- Condition of vessel wall
- normally not palpable
- in atherosclerosis, it can be felt as a cord between fingers and underlying bone.
- Character -various examples are given below:
slow rising pulse: (plateau pulse) low volume pulse, rises slowly and stays longer with the finger – aortic stenosis.
collapsing pulse: high volume pulse with normal upstroke but rapid downstroke – aortic regurgitation.
Pulsus bisferiens: two upstrokes in one beat – combined aortic stenosis and regurgitation (incompetence)
Pulsus paradoxus: pulse becomes weak/ impalpable during inspiration – cardiac tamponade, acute severe asthma
pulsus alternans: A strong beat alternates with a weak beat. – left ventricular failure, supraventricular tachycardia
pulsus bigeminus: strong and weak beats are coupled and followed by a longer pause – digoxin toxicity
Measurement of Blood Pressure:
The Blood Pressure is the product of the heart rate, stroke volume and peripheral resistance. There are two levels: systolic and diastolic.


There are two types of Sphygmomanometers (blood pressure apparatus) in common use.
- Mercury sphygmomanometer (more reliable)
- Aneroid sphygmomanometer
Methods of Measuring Blood Pressure
The patient should be relaxed, sitting or lying. Place the manometer at the same level as the cuff on the patient’s arm (Not necessary for aneroid type). The cuff should be wide enough to cover about two-thirds of the arm length. The length of the cuff should be 80% of the circumference of the limb and width should be 40% of the circumference of the limb. Remove all the clothing form the upper arm. Apply the cuff in such a way, that distance from the cubital fossa should be at least 1 inch.
Palpatory Method
Feel the radial pulse. Inflate the cuff to a pressure above the level at which the radial pulse becomes impalpable and then gradually deflate it. The level at which the radial pulse become palpable again is taken as the systolic pressure. It is a few mmHg less than the systolic pressure measured by the auscultatory method. Deflate the cuff completely.
Auscultatory method
Locate the tendon of biceps and palpate the brachial artery which lies on the medial side of it. Place the stethoscope over it and inflate the cuff above the systolic level determined by the palpatory method. Lower the pressure in the cuff by 5mmHg at a time. The level at which the Korotkoff sounds are heard for the first time is the systolic pressure. The Korotkoff sounds become louder as the pressure is lowered further; suddenly they become faint and then disappear. The level at which sounds disappear is the diastolic pressure.
Normal Blood Pressure:
- Normal: < 130/85
- High normal: 130-139/85-89
- Hypertension: 140/90
Pulse pressure:
It is the difference between the systolic and the diastolic pressure. Normal range is 30 – 60 mmHg.
Reference: Bedside Techniques – Muhammad Inayatullah | Shabbir Ahmed Nasir
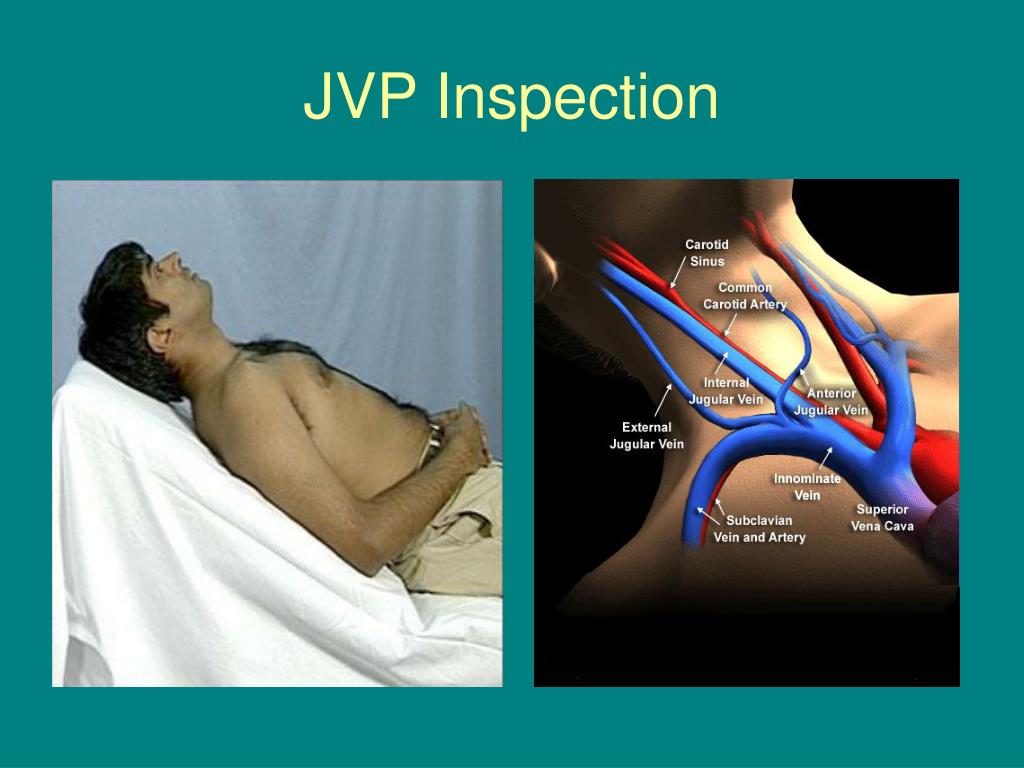
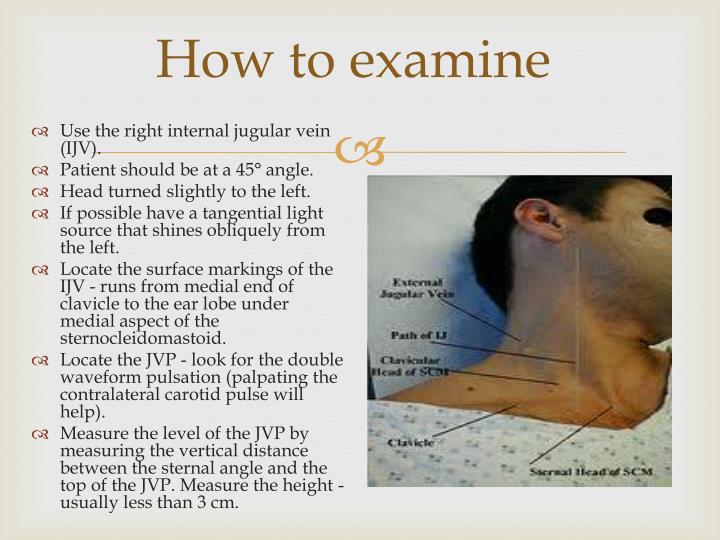
Examination of Neck Veins
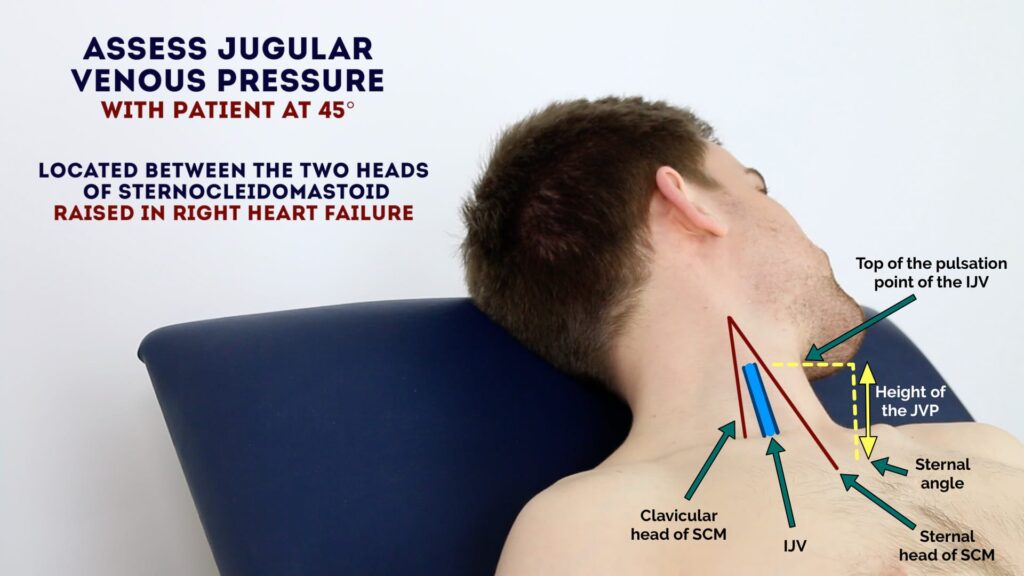
Central Venous Pressure is the same as the right atrial pressure. It is measured by inserting a catheter into the right atrium through the internal jugular or subclavian vein.
Jugular Venous Pressure (JVP) provides an indirect measure of central venous pressure. This is possible because the internal jugular vein (IJV) connects to the right atrium without any intervening valves, resulting in a continuous column of blood.
Normal mean right atrial pressure is 5 mm Hg, equivalent to 7 cm high column of blood.
As guessing the position of the center of right atrium might create confusion, it has become traditional to use the manubriosternal angle (angle of louis) as reference point for measuring the venous pressure. As normal mean pressure of the right atrium is 7 to 8 cm of blood, JVP more than 2 to 3 cm above the sternal angle is abnormal.

How to measure JVP?
Once the upper limit of venous pulsations has been determined, JVP is measured by two pencils?scales method. Place one pencil?scale at the central angle vertical to the ground and the other pencil/scale at upper limit of venous pulsations (transition point of distended and collapsed vein) in the neck, horizontal to the ground. Measure length of the vertical pencil (in cm) between the sternal angle and where it is crossed by the horizontal pencil. It is JVP; up to 3 cm is normal.
Causes of Raised JVP:
- Right Ventricular Failure
- Constrictive Pericarditis
- Pericardial Effusion
- Tricuspid Valve disease
How to examine Precordium?
Precordium is that part of the chest wall which overlies the heart and where heart sounds are heard. Examination of the precordium consists of following steps:
- Inspection
- Palpation
- Percussion Auscultation
- Auscultation
Inspection: Look for the following physical signs:
- Chest deformity (pectus excavatum or pectus carinatum)
- Bulging
- Scars (indicating past cardiac surgery)
- Pulsations
- Apex beat
- Parasternal border: due to Right ventricular hypertrophy
- Left 2nd Intercoastal space: dilation of pulmonary artery
- Right 2nd Intercostal space: due to aneurysm of aorta
- Pulsations in suprasternal notch: Aortic regurgitation
- Epigastrium: normally in thin individuals due to aorta. They could be due to right ventricular hypertrophy, pulsatile liver or aneurysm of abdominal aorta
- Prominent veins: superior vena cava obstruction
Palpation:
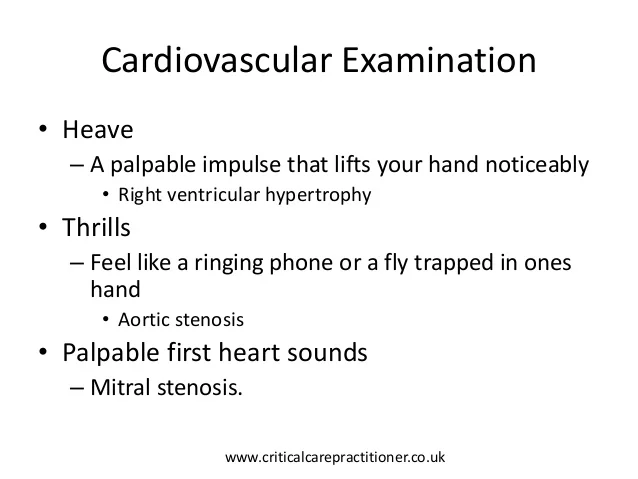
Palpate the precordium with the flat of the palm starting from the lower part of the left side of chest, then along the left parasternal border and finally upper part of the right side of the chest. Note the following physical signs:
- Apex Beat
- Left Parasternal heave
- palpable heart sounds
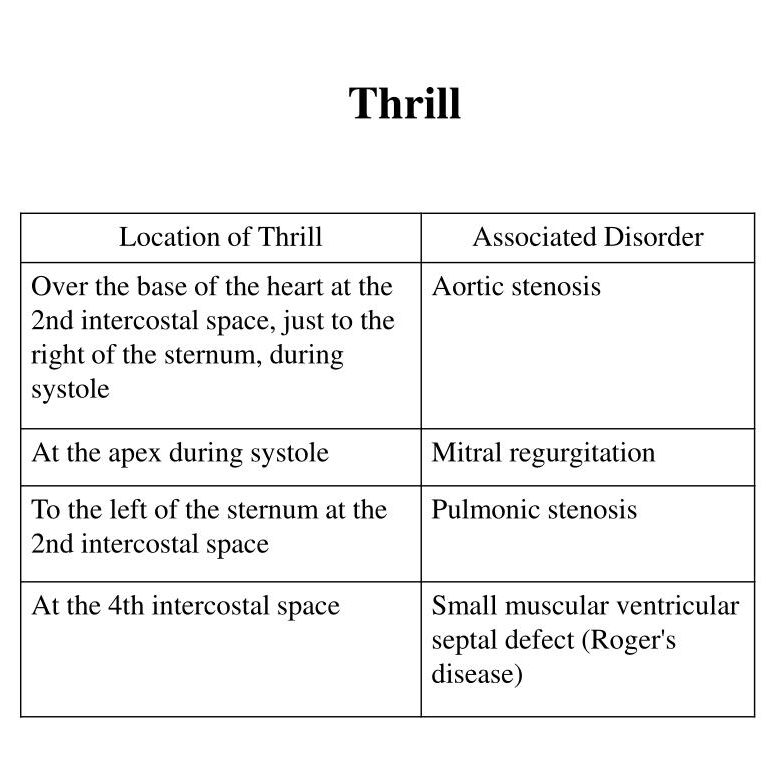
- Thrill
- Palpable pericardial rub
Causes of shift of Apex beat:
Cardiac Causes:
- Mitral regurgitation
- Aortic regurgitation
- Aortic stenosis
- ventricular Septal Defect
- Hypertension
- Ischemic Heart Disease
- Dilated Cardiomyopathy
Non cardiac causes:
- Deformities of the chest
- Pulmonary diseases causing shift of the mediastinum.
Causes of impalpable apex beat
- Thick chest wall
- Emphysema
- Pericardial effusion
- Dextrocardia

Percussion
Percussion of the precordium for cardiac dullness is not performed routinely nowadays due to chest radiograph, as it is a routine investigation and shows the exact size and shape of the heart. Normal cardiac dullness is medial to the mid clavicular line in the 4th intercoastal space.
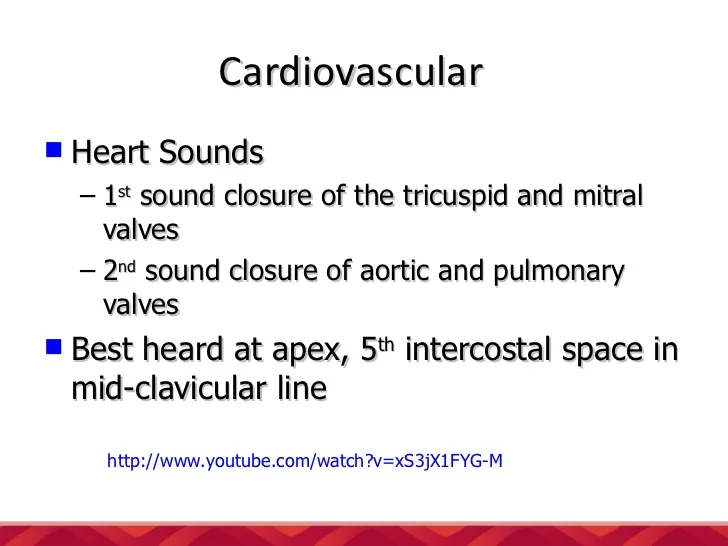
Auscultation
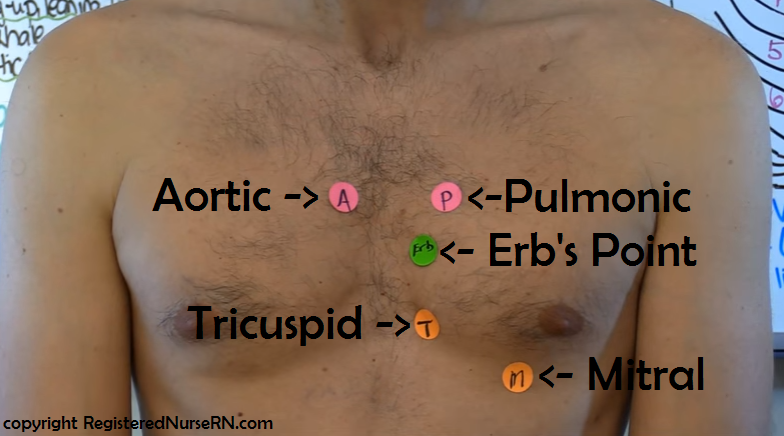
- Mitral Area corresponds to apex, where sound of mitral valve is heard
- Tricuspid area where sound of tricuspid valve is heard.
- Pulmonary Area is where sound of pulmonary valve is heard.
- There are two Aortic Areas, A1 (Right 2nd Intercoastal space close to the sternum) and A2 (left 3rd intercoastal space close to the sternum)
Method of Auscultation
- The areas mentioned above are useful for the description of clinical findings, Auscultate the whole of the precordium, not just the areas described. Auscultate whole of the precordium, either starting from the apex, moving up along the left parasternal border to the pulmonary area and then to the A1 area or starting from the A1 area and moving towards the apex.
- Auscultate in supine position, at first with the diaphragm and then with the bell.
- Turn the patient to the left lateral position and auscultate at apex with the bell for mid diastolic murmur of mitral stenosis.
- Ask the patient to sit up and lean forward and auscultate the pulmonary and A2 areas with the diaphragm. Patient should hold his breath on inspiration for murmur of pulmonary regurgitation and on expiration for murmur of aortic regurgitation.
During Auscultation, Note the following:
- Heart Sounds (first, second, third and fourth)
- Added Sounds (opening snaps, ejection systolic click, mid diastolic click, prosthetic valve sounds)
- Murmurs
- Pericardial Rub

