A 25-year-old lady one year history of episodic unilateral throbbing headache,
associated with nausea, vomiting and photophobia. There is a family history of
similar headaches. On examination, BP 120/80 mm Hg, pulse 80/min, no
neurological physical signs. Fundoscopy is normal. On investigations:
CBC: Hb 12.5 gm/dl, WBC 7×109, Platelets 235, ESR 20, contrast CT scan of head is
normal.
a) What is the most likely diagnosis and four precipitating factors of this type of
headache?
b) How will you manage her headache?
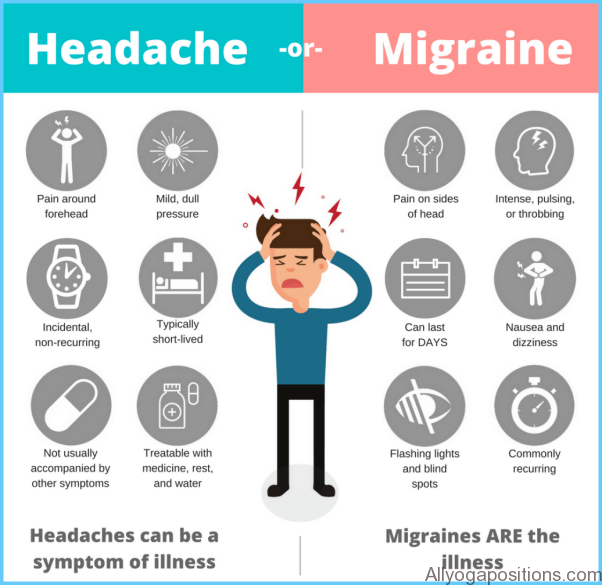
Migraine is defined as ‘A severe throbbing pain, generally experienced on one side of the head’. Migraine usually presents before the age of 40, affecting about 20% of females and 6% of males at some point in life.
The etiology is largely unknown. It is increasing evidence that it is due to dysfunction of ion channels. The headache phase is associated with vasodilatation of extracranial vessels.
Precipitating factors of Migraine headache
There is often a family history, suggesting a genetic predisposition. The female preponderance and tendency for some women to have migraine attacks in their menstrual period hints at hormonal influences. The contraceptive pill appears to exacerbate migraine in many patients. The dietary precipitants include cheese, chocolate or red wine. When psychological stress is involved, the migraine attack often occurs after the period of stress, like weekends or beginning of holiday.
Clinical features of migraine headache
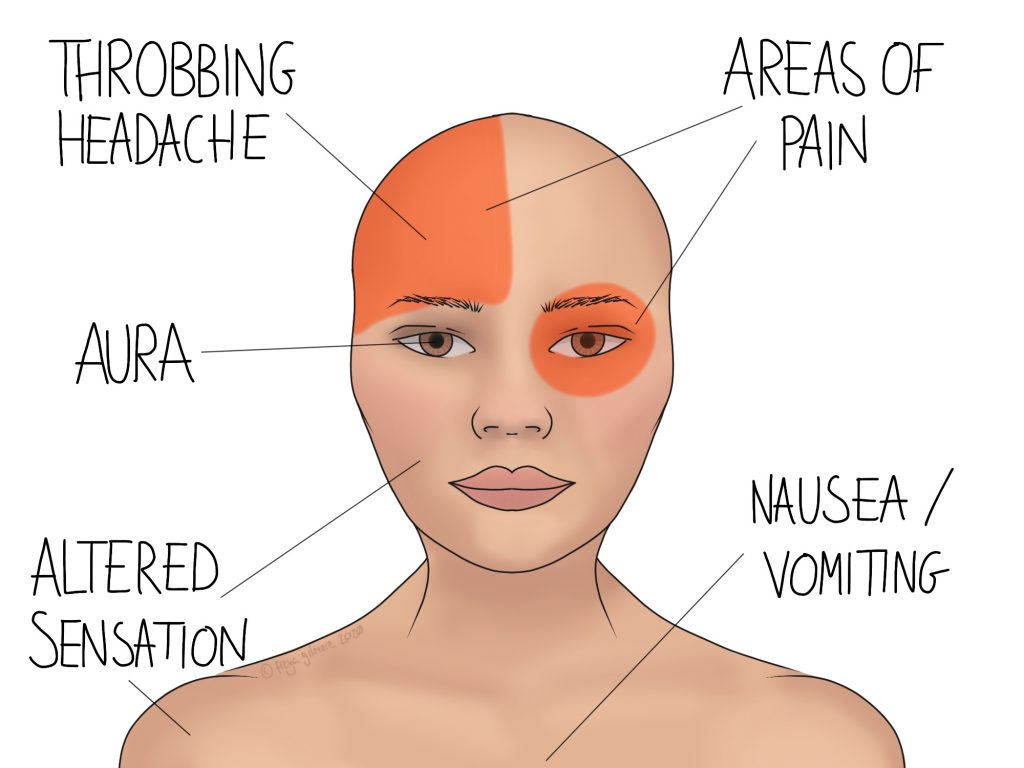
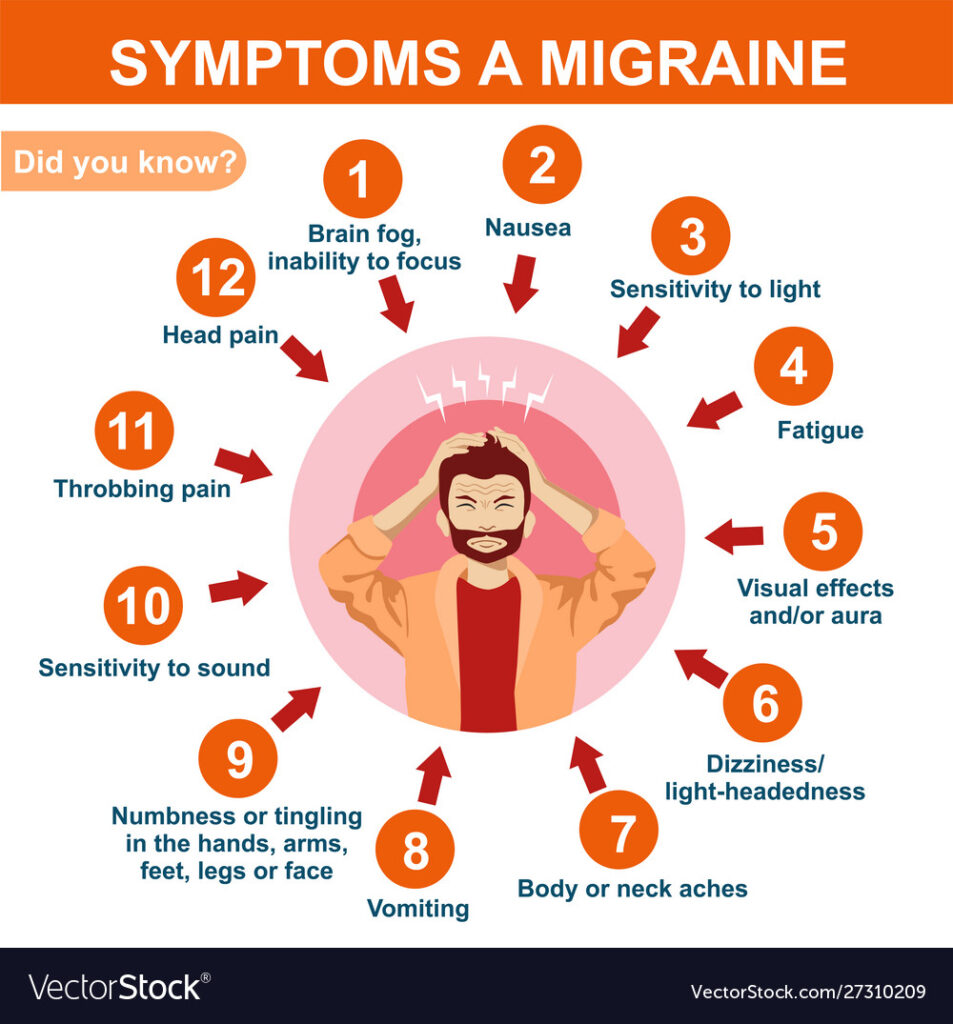
Migraine presents with a symptom triad of paroxysmal headache, nausea and/or vomiting, and an ‘aura’ of focal neurological events (usually visual).
Patients with all three of these features are said to have migraine with aura – ‘classical’ migraine.
Those with paroxysmal headache (with or without vomiting) but no ‘aura’ are said to have migraine without aura – ‘common’ migraine‘.
A non-specific prodrome of malaise, irritability or behavioral change may occur in the start of migraine. In ~20% of patients, migraine starts with aura. Shimmering, silvery zigzag lines march across the visual fields for up to 40 mins, sometimes leaving a trail of temporary field loss. Patients may feel tingling followed by numbness, spreading over 20–30 mins, from one part of the body to another. Dominant hemisphere involvement may cause transient speech disturbance (aphasia). Some 80% of patients have migraine without aura.
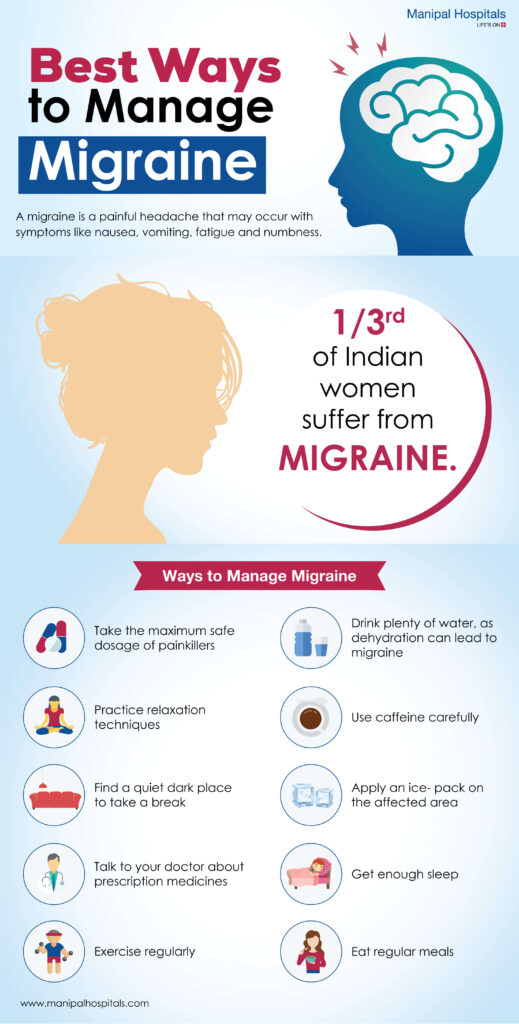
Management of migraine headache
Acute attack: Simple analgesia with aspirin or paracetamol, often with an antiemetic. Severe attacks can be treated with one of the ‘triptans’ (e.g. sumatriptan), 5-HT agonists that are potent vasoconstrictors of the extracranial arteries.
Prevention:
- Avoidance of identified triggers or exacerbating factors.
- If frequent, try calcium channel blockers, propranolol, amitriptyline or anti-epileptic drugs (e.g., sodium valproate).
- Women with aura should avoid estrogen treatment for contraception because of the risk of ischemic stroke.
- Long term use of codeine containing analgesic preparations should be avoided.
A 25-year-old lady one year history of episodic unilateral throbbing headache,
associated with nausea, vomiting and photophobia. There is a family history of
similar headaches. On examination, BP 120/80 mm Hg, pulse 80/min, no
neurological physical signs. Fundoscopy is normal. On investigations:
CBC: Hb 12.5 gm/dl, WBC 7×109, Platelets 235, ESR 20, contrast CT scan of head is
normal.
a) What is the most likely diagnosis and four precipitating factors of this type of
headache?
b) How will you manage her headache?
Reference: Davidson’s Principal and Practices, Davidson’s essential of Medicine
Click here to see Next; Emergency Drugs you should know About

